Dutch scientists are theorizing that mesothelioma can be beaten by upsetting the balance between macrophage types found in each mesothelioma tumor.
Macrophages should be seen as a therapeutic target in the treatment of malignant pleural mesothelioma, contend the researchers from Erasmus MC Cancer Institute in Rotterdam, The Netherlands, in the peer-reviewed online journal PLOS ONE.
They assert that changing the macrophage ratio within the tumors would be particularly effective in patients with the epithelioid form of mesothelioma.
Mesothelioma Cells Targeted
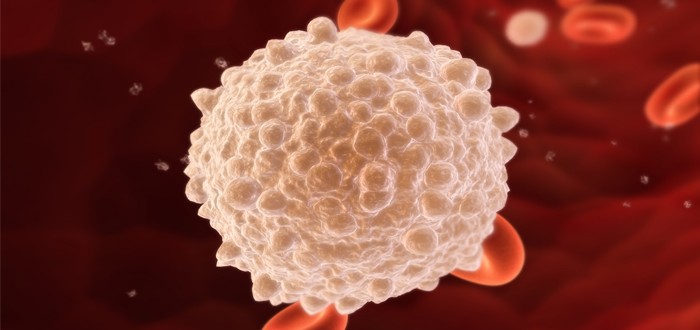
Macrophages are white blood-cells that conduct search-and-destroy missions against bodily invaders, such as cancer.
Phagocytosis is the technical term used by guys in lab coats to describe what macrophages do.
The researchers from Erasmus explain that up to two-thirds of a tumor’s mass are macrophages the tumor has drawn into battle.
These are known as tumor-associated macrophages, or TAMs.
TAMs come in two varieties. They go by the names M1 and M2. In a patient who has mesothelioma, M1 macrophages are the good guys and M2 macrophages are traitors.
The reason is that the M1 macrophages spend all their time chipping away at mesothelioma cells, trying to scuttle them.
M2 macrophages, on the other hand, are not supposed to be allies with mesothelioma. They are supposed to be helping the M1s. But somehow, mesothelioma tricks them into assisting the enemy.
The problem is that M2 macrophages prove to be quite effective at helping mesothelioma. And, unfortunately, there typically are many more M2s than M1s in the combat zone.
With the M1s outnumbered and outgunned, the mesothelioma tumors grow and gobble up territory fast.
The researchers believe that it is possible to shift this ratio so that there are far more M1s than M2s. If this shift can occur, mesothelioma tumors will receive less help and be more vulnerable to destruction.
Mesothelioma Survival Was Original Focus
The researchers started off with a different aim. They wanted to see if the natural ratio of M1s to M2s could be used to predict mesothelioma survival following extrapleural pneumonectomy surgery.
Eventually, the researchers came to the conclusion that the macrophage balance was not a reliable predictor of mesothelioma surgery outcomes.
But they were heartened to discover that it could be used reliably to predict overall mesothelioma survival.
The research involved looking in depth at tumor specimens obtained from eight malignant pleural mesothelioma patients. The patients had undergone mesothelioma surgery plus chemotherapy.
The tumors from these eight were compared to tumors from another eight mesothelioma patients who had received just chemotherapy, no surgery.
In both sets of patients, the researchers calculated how many macrophages were contained in each tumor specimen prior to treatment. Then they calculated the number again after treatment.
Comparing the two, they found the difference wasn’t meaningful enough to help predict whether the surgery would extend the lives of the mesothelioma patients who underwent it.
Nonetheless, they did find the difference of sufficient significance to let them make predictions about overall mesothelioma survival.
From there, by connecting the dots, they realized that it also might be possible to produce a favorable shift in the ratio of M1s to M2s.
Whether it can be done remains to be seen. It will no doubt be the subject of much additional research in the future.